An ovarian cyst is a fluid-filled sac that forms on or within an ovary. These cysts come in different sizes and can arise from various causes. Although numerous ovarian cysts are benign and might remain asymptomatic, certain cysts can produce symptoms or lead to complications, necessitating medical assessment and intervention.
While most ovarian cysts are benign and pose no threat, their size and origin can vary. While some ovarian cysts remain asymptomatic, they can become problematic if they enlarge, rupture, or cause discomfort.
These cysts are frequently observed in women of childbearing age, often forming during the ovulation process. Their incidence tends to decline post-menopause. Many times, they dissipate on their own without evident symptoms or necessitating intervention. Yet, in certain situations, they might signal an underlying medical issue and could require surgical removal.
Although it’s challenging to entirely prevent ovarian cysts, certain precautions can mitigate the risk. These include maintaining a healthy weight, opting for contraception, and undergoing routine pelvic exams.
Incidence of ovarian cyst in Nepal
The exact prevalence of ovarian cysts in women remains uncertain, largely because many cases are asymptomatic and go undiagnosed.
By the age of 65, about 4 out of every 100 women will have been hospitalized due to ovarian cysts. In a study involving 335 asymptomatic women aged 24 to 40, 8% were found to have an adnexal lesion. An adnexal lesion refers to a growth, either fluid-filled or solid, located around the ovaries, fallopian tubes, or adjacent connective tissue.
Among postmenopausal women, 2.5 out of every 100 have a simple unilocular adnexal cyst, typically benign and often resolving on its own.
In a comprehensive survey of 33,739 women spanning both premenopausal and postmenopausal stages, nearly half displayed an adnexal cyst on transvaginal ultrasound. Of these, approximately 63.2% (or 9,958 women) showed cyst resolution upon subsequent ultrasounds.
Types of ovarian cyst
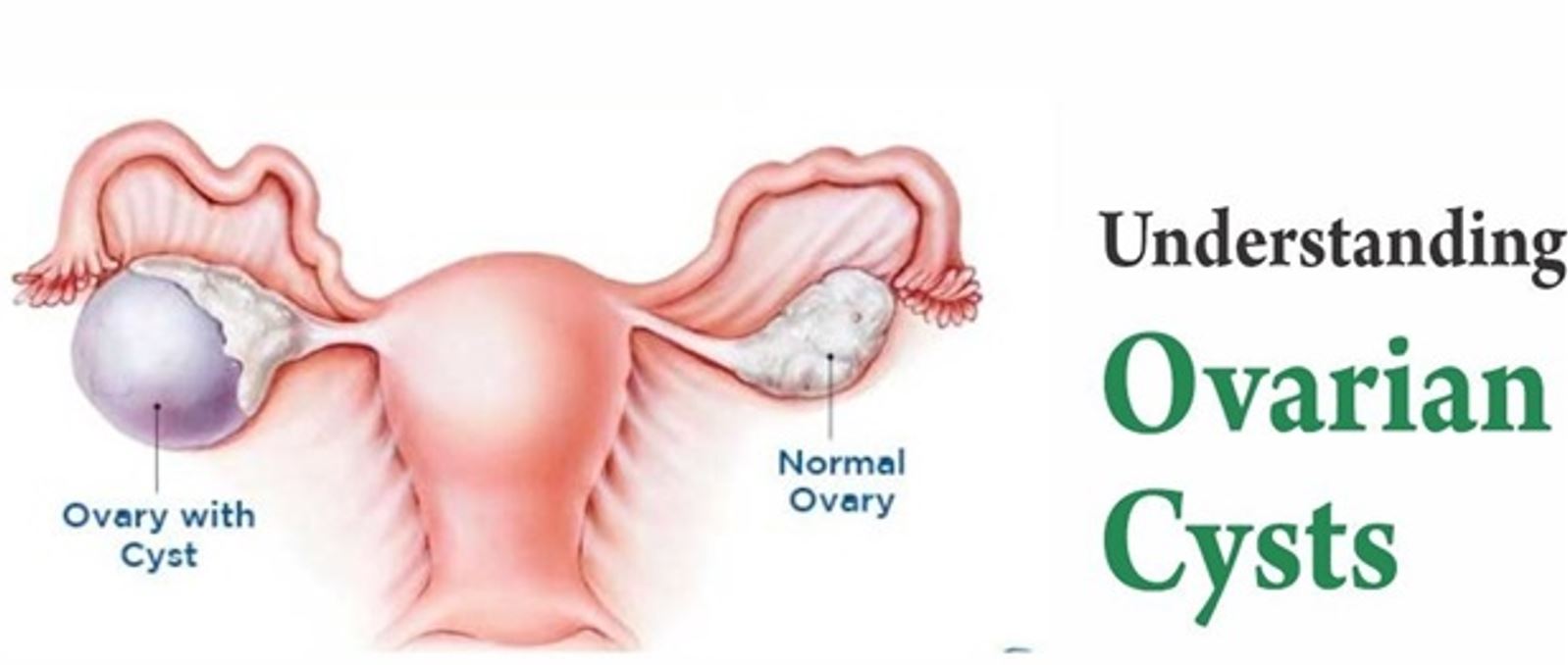
Women possess two ovaries situated on either side of the uterus in the pelvic region, integral to the reproductive system. If a cyst emerges on the left ovary, it’s termed a left ovarian cyst; conversely, if it arises on the right ovary, it’s called a right ovarian cyst. Occasionally, cysts, known as bilateral ovarian cysts, can manifest on both ovaries simultaneously.
Ovarian cysts can be broadly classified into two categories:
1. Functional ovarian cysts
These are the most prevalent benign ovarian cysts, typically transient and indicative of a healthy ovulatory cycle. Typically, they diminish within approximately two months without intervention.
– Follicular Cysts: These arise when a follicle, intended to release an egg during ovulation, doesn’t do so and instead accumulates fluid, enlarging in the process.
– Corpus Luteum Cysts: Post-ovulation, the follicle becomes the corpus luteum. On occasion, fluid accumulation within the corpus luteum can give rise to cysts.
Both follicular and corpus luteum cysts can occasionally transform into hemorrhagic cysts due to ruptures, injuries, certain medications, or ovulation-related factors. Treatment options encompass rest, pain relief, and surgical intervention if the cyst is substantial and symptomatic.
2. Pathological Cysts:
These are less common and stem from various medical anomalies.
– Dermoid Cysts: These are unique growths containing diverse bodily tissues like skin, teeth, hair, and occasionally, brain matter. Symptoms may be absent until the cyst reaches a considerable size. Their origins can be attributed to infections, genetic anomalies, or developmental irregularities.
– Endometriomas (Chocolate Cysts): These cysts are replete with endometrial tissue, mirroring the tissue shed during menstruation. Manifestations include intense menstrual cramps, non-menstrual pelvic discomfort, and potential infertility.
– Cystadenomas: These growths surface on the ovary and can contain either a watery or a thicker, mucoid fluid.
– Polycystic Ovary Syndrome (PCOS): This hormonal imbalance prompts the formation of numerous small cysts on the ovaries, leading to their enlargement.
– Ovarian Cancer Cysts: Distinct from the aforementioned conditions, these are solid formations comprising malignant cells, not fluid-filled sacs.
Symptoms of ovarian cysts
Many women may harbour ovarian cysts without evident symptoms. Typically, symptoms manifest when a cyst ruptures, enlarges significantly, becomes twisted, or impedes ovarian blood flow. When symptomatic, manifestations can range in intensity and might comprise:
- Pelvic Discomfort: Ovarian cysts often induce sensations of pressure or pain in the lower abdominal region. This can vary from a mild, persistent ache to intense, intermittent sharp pains. A ruptured cyst may result in pronounced, acute pain, while a hemorrhagic cyst can present with sudden, intense pelvic discomfort on its affected side.
- Abdominal Distention: Certain women might feel a consistent or sporadic sensation of abdominal fullness, swelling, or bloating due to ovarian cysts.
- Menstrual Irregularities: Cysts that secrete hormones can disrupt the menstrual cycle. Notably, endometriomas or “chocolate cysts” associated with endometriosis can exacerbate menstrual pain.
- Unexplained Weight Fluctuations: Ovarian cysts, notably in conditions like PCOS, can be correlated with weight changes and challenges in weight management.
- Fertility Challenges: While the presence of a singular cyst typically doesn’t impact fertility, conditions like PCOS, characterized by multiple cysts, can potentially diminish fertility prospects.
- Organ Displacement: Enlarged cysts can exert pressure on neighbouring organs like the bladder or rectum, leading to heightened urinary urgency, dysuria, constipation, or altered bowel patterns.
- Painful Intercourse: Particularly sizable cysts, when ruptured, can cause acute pain during sexual activity, often due to penile pressure.
- Gastrointestinal Symptoms: A cyst’s torsion or rupture might induce nausea, vomiting, and abdominal discomfort.
- Concerning Signs: Symptoms suggestive of a malignant cyst include persistent bloating, pelvic discomfort, altered bowel movements, early satiety, and irregular menstrual bleeding.
Causes of ovarian cysts
The precise origin of many ovarian cysts remains elusive. However, several factors, including menstrual cycle regularity, may influence their formation.
- In premenopausal women, the predominant causes of ovarian cysts encompass:
- Hormonal Imbalances: Disturbances in hormones governing the menstrual cycle can pave the way for cyst development.
- Polycystic Ovary Syndrome (PCOS): This condition is marked by excessive production of hormones like testosterone, fostering the emergence of multiple ovarian cysts.
- Thyroid Disorders: Both hyperactive and underactive thyroid conditions can disrupt ovulation. The resemblance between the alpha subunit of thyroid-stimulating hormone (TSH) and hCG might promote ovarian and cyst growth in hypothyroidism.
- Endometriosis: Advanced stages of endometriosis can lead to the formation of endometrioma cysts, colloquially termed “chocolate cysts.”
- Pregnancy: In early gestation, ovarian cysts may develop to sustain the ovary until placental formation, occasionally persisting into later pregnancy stages.
- Pelvic Infections: Severe infections can extend to the ovaries and fallopian tubes, resulting in cysts filled with pus in proximity to these structures.
- Medications: Certain fertility treatments and hormone replacement therapies can elevate the propensity for ovarian cyst development.
- Genetic Factors: Some ovarian cysts may have genetic underpinnings, with individuals having a familial predisposition to ovarian cancer being at an augmented risk.
- Ovarian Cancer: While rare, some ovarian cysts in premenopausal women may be indicative of ovarian cancer, albeit accounting for less than 1% of ovarian growth.
- For postmenopausal women, the leading causes of ovarian cysts include:
- Non-Malignant Growths
- Accumulation of Fluid within the Ovary
- Ovarian Cancer: New growths in or around the ovaries are more likely to be malignant compared to menstruating counterparts.
Diagnosis of ovarian cyst
The assessment of an ovarian cyst typically encompasses a thorough review of the patient’s medical history, a physical examination, and specialized diagnostic procedures by an experienced Gynecologist. Here’s a breakdown of the diagnostic steps for ovarian cysts:
1. Medical History: Gathering detailed information about the patient’s symptoms, menstrual cycle, previous medical conditions, and family history.
2. Imaging Studies: Ultrasound – Abdomen & Pelvis, Transvaginal Ultrasound (probe is inserted into the vagina for closer examination). Pelvic MRI also provides a comprehensive view of the pelvic region, aiding in the identification and characterization of ovarian cysts.
3. Pathological Tests: Complete Blood Count (CBC), Pregnancy Testing beta HCG, Urinalysis, Swab Test, Cancer Antigen 125 (protein often elevated in ovarian cancer, Cyst or in other related conditions).
Treatment of ovarian cyst
Non-surgical Treatment Options for Ovarian Cysts: Treatment approaches for ovarian cysts are tailored based on factors such as the patient’s age, menopausal phase, cyst size, and any suspicious characteristics indicating possible malignancy.
Here are some common strategies for managing ovarian cysts:
- Watchful waiting (Observation): Many cysts in reproductive-age women, such as follicular or corpus luteum cysts, are benign and often disappear within a couple of months. While they might rupture and cause discomfort, they usually resolve spontaneously. A gynaecologist might advise regular monitoring without immediate intervention.
- Pain management: For cyst-related discomfort, medications like Nonsteroidal anti-inflammatory drugs (NSAIDs) or stronger pain relievers may be prescribed to alleviate symptoms. Make sure medicine is taken under the gynecologist’s guidance.
- Oral contraceptives (Birth Control Pills): To minimize the risk of functional ovarian cysts, contraceptive pills can be recommended. By regulating hormone levels and preventing ovulation, they can deter the formation of such cysts. For those experiencing recurrent cysts or seeking preventive measures, oral contraceptives might be a suitable option.
- Cyst drainage/surgical intervention: In cases where a cyst is particularly large or painful, it can be drained using a needle or a minor surgical procedure. However, it’s important to note that this method may not offer a permanent solution, as the cyst could reform over time.
For patients with simple ovarian cysts, aggressive treatment isn’t always necessary since these cysts often resolve independently.
Ovarian cyst prevention:
While it’s challenging to completely prevent ovarian cysts, adopting certain practices can potentially lower the risk of their development:
- Regular Health Checkups: Periodic visits to a gynaecologist can aid in overseeing reproductive health, and facilitating early detection and management of any cysts.
- Maintaining a Healthy Weight: Obesity is linked to an increased risk of ovarian cysts. Thus, embracing a balanced diet and engaging in regular physical activity can mitigate this risk.
- Balanced Diet: Consuming a nutritious diet not only supports weight management but also guards against other chronic ailments like cardiovascular diseases, stroke, and type 2 diabetes.
- Regular Exercise: Engaging in consistent physical activity can bolster both physical and hormonal health.
- Avoiding Harmful Habits: Steering clear of smoking and limiting alcohol intake is pivotal as these habits can compromise ovarian health and elevate cyst risk.
- Cautious Hormone Use: Be careful with hormone therapies, as their excessive use can influence the onset of ovarian cysts.
Additional Recommendations:
- Incorporate Fruits and Veggies: These foods are teeming with antioxidants and essential nutrients that shield cells from harm.
- Moderate Processed Foods and Sugary Beverages: These items, rich in calories, unhealthy fats, and sugars, can contribute to obesity and other health issues, including ovarian cysts.
- Prioritize Sleep: Adequate sleep is vital for overall well-being. Inadequate sleep can escalate cortisol (stress hormone) levels, potentially heightening health risks.
- Stress Management: Chronic stress can disrupt hormonal balance, increasing susceptibility to ovarian cysts. Implementing stress management techniques is pivotal for holistic health and cyst prevention.
Ovarian cysts and pregnancy
Ovarian cysts can manifest during early pregnancy, even in the absence of menstrual cycles. Typically, these cysts pose no significant threat, mirroring the benign nature of most ovarian cysts.
Nevertheless, if these cysts persist and enlarge during pregnancy, potential complications such as rupture, torsion, or childbirth challenges could arise. Hence, maintaining regular consultations with a gynaecologist throughout your pregnancy and beyond is crucial.
For those with polycystic ovary syndrome (PCOS), there’s an elevated likelihood of encountering complications like gestational diabetes, hypertension during pregnancy, miscarriage, or preterm birth.
Engage in a discussion with your gynaecologist regarding your specific risks and available treatment avenues. They will offer comprehensive guidance and tailor recommendations to ensure the most optimal and healthy pregnancy outcome for you.

